(Part I is here, and part III is here)
In certain respects, development of the view that embodied experience is crucial to understanding the mind and brain reached a nadir in the period after World War II, at least within psychology. Behaviorism had redefined psychology as an “objective” science with no need to refer to consciousness or phenomenology. There was continuation of phenomenological research from the German gestalt psychologists, but it was not until after World War II that clinically-oriented humanistic psychology explicitly articulated the need for more holistic, “person-centric” perspectives emphasizing existential concerns: the search for meaning, the experience of health and illness, emotions, and consciousness.
While many philosophers in Europe continued to develop phenomenology, Contintental philosophy was increasingly concerned with logical positivism, which emphasized that many traditional problems could be solved through formal logic, and those not approachable in this way were suspect. Formal logic reached a apotheosis of sorts with the advent of computers, a class of systems having internal memory storage and symbolic-logical operations, and with them came a number of seminal figures that transformed models of mind and brain. In particular, Norbert Weiner‘s (1894-1964) meta-discipline of cybernetics, Claude Shannon‘s (1916-2001) information theory, Alan Turing‘s (1912-1954) and John von Neumann‘s (1903-1957) canonical work on computation, Jean Piaget‘s (1896-1980) theories of the sequential process by which infants and small children learn language and perception in stages, all resulted in an explosion of new perspectives on cognition, language, memory, perception, problem-solving. By the late 1950’s the overlapping field(s) of artificial intelligence (AI) and cognitive science got the attention of researchers in psychology, linguistics, philosophy of mind, neuroscience, anthropology, therapy, and organizational management. Herbert Simon (1916-2001) modeled human problem solving in the face of uncertain information, and co-developed what became known as general systems theory, and along with Allen Newell (1927-1992) developed automated theorem-provers and chess-playing programs. Noam Chomsky‘s investigation of the symbolic logical rules underlying grammar and syntax generated an attack on environment-produced behaviorist theories of language, the flaws of which dramatically came to a head in the North Texas Symposium on Language in 1959.
While the door to explaining psychological phenomena in terms of mental categories and concepts had been re-opened, these new models generally formulated explanations in terms of impersonal information-processing and rule-based symbolic-logical theories of non-conscious aspects of the mind. These new “cognitivists” had absorbed certain scruples from the behaviorists, and typically disdained concepts such as “consciousness” in their models of the mental processes. Cognitivism remained “system-centric”, not person or body-centered, and focused on reducing mental activity to computational,information-processing and representational processes. There was a general lack of interest in using various first-person, introspection-based methods such as those of William James, or Edmund Husserl, though cognitivism and behaviorism alike asked subjects for verbal reports within experiments.
However, clinical neurologists continued to advance an approach to psychological and cognitive phenomena that reflected a richer and broader understanding of the mind. The First and Second World Wars provided a huge pool of subjects with specific localized lesions and corresponding deficits in memory, speech, motion, etc. The Russian neurologist Alexander Luria (1902-1977) spent about 30 years with a patient, the soldier Zazetsky, who sustained a bullet wound to his left occipito-parietal cortex. Zazetsky’s struggle to use journal writing cope with being unable to remember new events is described in The Man With a Shattered World (1972) as a fight “to live, not merely exist.” Zazetsky wrote: “I’m in a fog all the time…. All that flashes through my mind are images…hazy visions that suddenly appear and disappear.”

Taking the long view of the development of a science of the mind, the praxis-driven demands of the clinic balanced somewhat the behaviorist and cognitivist disavowal of consciousness as a research topic. Focusing on the struggle of a brain-injured patient to live meaningfully meant that at least a small part of the ever-more fragmented field of psychology overtly or implicitly emphasized embodied and conscious aspects of cognition. It should be emphasized that a division of labor was in effect. Clinicians deal with people, while cognitive scientists deal with systems. As neurologists and psychologists published case studies, the more theoretically minded extrapolated from these reports to highlight an understanding of human mental functioning that did not exclude consciousness and the existential, personal, meaningful dimensions of experience that are grounded in the lived body.
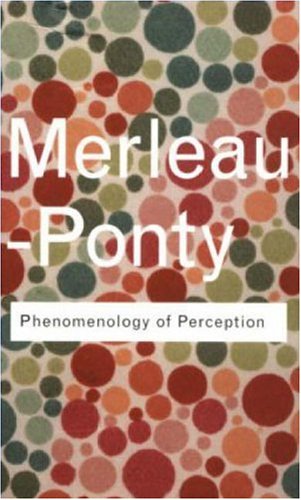
Across the ocean, in France, while structuralism began to dominate intellectual life after World War II, developments in phenomenological research continued apace. Most imprtantly was the philosopher Maurice Merleau-Ponty (1908-1961) analyzed and critqued the phenomenology of the philosopher/mathematician Edward Husserl. Foregoing Husserl’s hugely ambitious project of project of providing the most rigorous epistemological foundation possible for science and philosophy through investigations into experience, Merleau-Ponty attempted to reintegrate the penetrating Husserlian observation analysis of conscious phenomena into the structure of how consciousness is grounded and lived out bodily.
Phenomenologist Maurice Merleau-Ponty
- This change of emphasis allowed a bridge towards grasping how the lived body is related to the objectively-described physical body of physiology, behaviorism, and brain science. Works such as The Structure of Behavior and The Phenomenology of Perception are tantalizing hints that had Merleau-Ponty lived a long life, neurophenomenology might have emerged decades before the 1990’s. Merleau-Ponty articulated a post-Cartesian view of the mind that subverted the subject-object split. He used the notion of co-constitutionality to grapple with the enigmatic coupling and engagement of embodied mind to the world. Two quotes from The Phenomenology of Perception are appropos (pg. 407):
“Inside and outside are inseparable” (pg. 407)
“Insofar as I have hands, feet; a body, I sustain around me intentions which are not dependent on my decisions and which affect my surroundings in a way that I do not choose” (pg. 440)
Those psychiatrists and psychologists who attempted to apply the insights of Husserl, Martin Heidegger (1889-1976) and Merleau-Ponty especially developed what became known as phenomenological psychology. Heidegger gave lectures to physicians about ontology,while Ludwig Binswanger (1881-1966) and Medard Boss (1903-1990) attempted to apply his analysis of dasein (“being-there”) to clinical contexts. Phenomenological psychology showed a pronounced clinical influence from a key synthesizer of the neurological and phenomenological research traditions: the neuropsychiatrist Erwin Straus (1891-1975, who was possibly the first neurophenomenologist.
Erwin Straus, MD: the first neurophenomenologist?
He is quoted in Man, Time, and World: Two Contributions to Anthropological Psychology (1982) as stating:
“The physiologist, who in the everyday world relates behavior and brain, actually makes three kinds of things into objects of his reflection: behavior, the brain as macroscopic formation, and the brain in its microscopic structure and biophysical processes. From the whole-the living organism-the inquiry descends to the parts: first of all to an organ-the brain-and finally to its histological elements. Statements concerning the elementary processes acquire their proper sense only in reference back to the original whole”
Probably the best known exponent of a phenomenogical approach to clinical psychology and psychiatry was RD Laing (1927-1989), who in 1965 wrote a classic case-study analysis of the experience of schizoids in The Divided Self: an existential study in sanity and madness. In it he describes one patient:
“Julie’s self-being had become so fragmented that she could best be described as living a death-in-life existence in a state approaching chaotic nonentity.
In Julie’s case, the chaos and lack of being an identity were not complete. But in being with her one had for long periods that uncanny ‘praecox’ feeling described feeling’ described by the German clinicians, i.e. of being in the presence of another human being and yet feeling that there was no one there. Even when one felt that what was being said was an expression of someone, the fragment of a self behind the words or actions was not Julie. There might be someone addressing us, but in listening to a schizophrenic, it is very difficult to know ‘who’ is talking, and it is just as difficult to know ‘whom’ is addressing.”
In the 1970’s and early 1980’s, neurologists like Oliver Sacks continued in the neuropsychological tradition of Luria, and documented the existential struggles of patients with brain disorders. In 1970 he produced an eminently readable, phenomenologically rich classic of neuropsychology: The Man Who Mistook His Wife for a Hat. He wrote persuasively that while there are indeed computer-like aspects of the brain, the cognitive, computationalist or information-processing model nonetheless does not address the full spectrum of human psychological reality (pg. 20):
“But our mental processes, which constitute our being and life, are not just abstract and mechanical, but personal, as well.”

The European-flavored, humanistic field of phenomenological psychology (also called existential-phenomenological psychology) offers an alternative for researchers dissatisfied with mechanistic cognitivitism, behaviorism and physiological psychology. However, as far as I can tell, after the passing of Erwin Straus, phenomenological psychology has had little or no interest in cognitive neuroscience. The major exception to this I can find was in 1981, when phenomenological/biophysiological psychologist Donald Moss and cognitive neuroscientist Karl Pribram each wrote fascinating essays on comparing brain science and phenomenology in the collection The Metaphors of Consciousness (Valle and von Eckartsberg, Eds). This is of historical interest as an early instance of an explicit dialoug between neuroscience and existential-phenomenology.

Pribram’s essay “Behaviorism, Phenomenology, and Holism in Psychology” pointed to the need for a broader, phenomeologically and neurobiologically informed approach to psychology (pg. 142:
“But there are limits to understanding achieved solely through the observation and experimental analysis of behavior. These limits are especially apparent when problems other than overt behavior are addressed, problems related to thought or to decisional processes, to appetive and other motivational mechanisms, to emotions and feelings, and even to images and perception”.
and (pg. 146):
“Existential-phenomenological psychology has not, up to now, been very clear in it’s methods. I suggest that multidimensional analyses (factor analysis, principle components analysis, stepwise discriminant analysis) might serve well as tools to investigate the structure of experience-in-the-world.”
Moss lucidly analyzed the similarities and divergences between neuroscience and existential-phenomenology in a essay entitled “Phenomenology and Neuropsychology” (pg.159):
“Pribram points to the role of the brain processes in”constructing” the world as perceived. Yet existential-phenomenology has also emphasized the “constituting functions”of the ego (Husserl), the constituitive role of the lived body (Merleau-Ponty), and the role of the human body and upright posture in articulating the world of sensory experience (Straus). Thus, neither school of thought naively recognizes a reality per se unaffected by the presence and condition of the organism. ”
Such exchanges occurred on the margins of mind-science. By the 1960’s, the largely cold-war funded research program of Artificial Intelligence (A.I) and growing interest in cognitive or information-processing approaches to problems in psychology etc. had produced a “cognitive revolution”. Some brave cognitivists even made use of introspective techniques (though not without drawing fire from behaviorists). Herbert Simon asked his subjects to verbally report on how they solved logic-puzzles, much to the chagrin of the remaining orthodox behaviorists. The renewal of mentalistic language and willingness to freely use data from introspection and verbal reports from subjects about how they solved logic problems was a robust challenge to the behaviorists, but over time a rapprochement ensued.
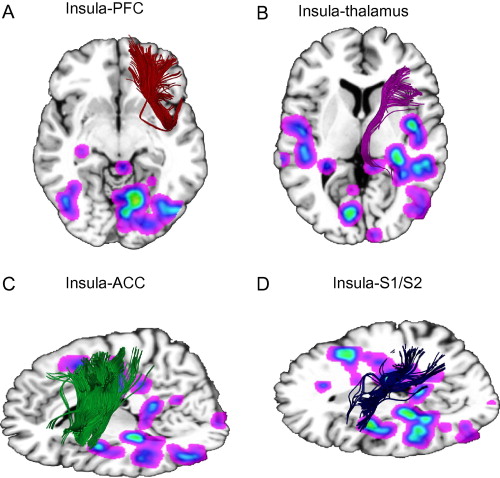
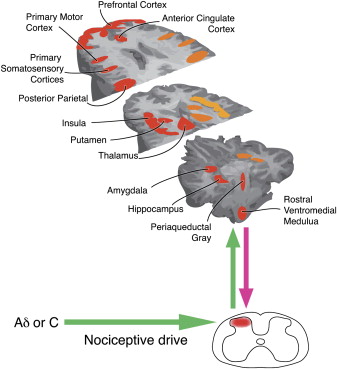
But what really allowed the scientific study of consciousness and experience to re-emerge was the success of theoretical and laboratory neuroscience. EEG data had been produced for years with good temporal but limited spatial resolution, but in the 1970’s and 1980’s an alphabet soup of new imaging technologies (CAT, PET, MRI, and recently MEG) allowed neuroscientists to better “peek inside” the living brains of subjects in experiments. Progress in molecular biology, genomics, and biophysics in the postwar West allowed curious researchers to formulate models of emotions in chemical terms, such as the finding of endogenous opiates (or endorphins) and their receptors in the brain. The finding that nerve fibers connect with the organs of the immune system helped ground theories of the effect of emotions and beliefs on health, leading to the interdiscipline of psychoneuroimmunology. A growing industry to synthesize pharmaceutical products based on the molecular structure of receptor proteins has led to neuropharmacology and neuropsychopharmacology.
Some brain researchers looking for theoretical models of the mind found the information-processing/computationalist approach of the cognitivists limiting in understanding emotions and experience. Cognitive science itself had been rocked from its early (late 1950’s-early 1960’s) success to the gradual realization that many aspects of mind are not easily characterized as formal-logical, rule-based systems, as had been predicted by the phenomenologically-informed philosopher Hubert Dreyfus (1972) in What Computers Can’t Do, where he argued that rule-based, symbolic-logical, representationalist models of mind and language fail to deal with the radically embodied nature of cognition. This was hotly rejected by prominent AI researchers, but later influenced Terry Winograd, among others.

Mostly the insights of clinical neurologists and phenomenological psychologists were ignored in postwar cognitive science, which had a great overlap with computer science and Artificial Intelligence (A.I). Indeed, cognitivists and AI engineers might profess agnosticism about the neurobiology of the mind, viewing brain “hardware” as the domain of other specialists. In the late 1950’s and through the 1960’s, cognitive science and Artificial Intelligence seemed to have revolutionary new insights. AI as engineering of useful artifacts overlapped with AI as cognitive modeling. An early era of exciting optimism eventually gave way to slow progress on “general purpose” problem solving. The limitations of their symbolic-logical, information-processing, and computationalist approach led others to develop the hybrid field of cognitive neuroscience. Sometimes there were interesting discrepancies between the two: onetime “pure” cognitivist Stephen Kosslyn performed neuroimaging experiments on subjects who were asked to rotate mental objects. According to John McCrone’s report of Kosslyn’s work in Going Inside: A Tour ‘Round a Single Moment of Consciousness, the resulting pattern of distributed activity across disparate brain regions was difficult to reconcile with the neat schematic Kosslyn had developed as an abstract cognitive model possessing a few modules for accomplishing aspects of the rotation operation. This lends credence to those who propose that cognitive science must be much more thoroughly integrated with the “gory details” of neuroscience, with the neural networks/connectionist camp serving as a conceptual bridge fro brain to symbols and representations. Over time, the lack of interest in biology and “implementation agnosticism” of some computationalist cognitive scientists has given way to modern cognitive neuroscience. A movement in the 1980’s to reform cognitive science and artificial intelligence along biologically-inspired and “subsymbolic” lines known as connectionism, artificial neural-networks, and parallel-distributed processing splits cogntivism to this day.
A pathbreaking (and for some, puzzling*) book appeared in the second half of the 1980’s that seemd to point the way to a synthesis of neurobiology, cognitivism, computer science, and phenomenology: Understanding computers and cognition: a new foundation for design by AI and language-processing expert Terry Winograd and Fernando Flores:

The book proposed a phenomenologically-grounded understanding of how people in real-world environments use systems that software designers build. It took inspiration from Humberto Maturana and Francisco Varela‘s idea of autopoesis, a cybernetics-inspired, dynamical theory of organisms self-organizing their own structure by regenerating parts and by being coupled to their environment, until death. The brains of creatures do not represent features (such as colors) of objects external to them as cognitivists typically assume. Rather, each ecologically-situated animal brings forth or co-constitutes a perceived world through evolutionarily-selected sensorimotor systems. Autopoesis is a sort of post-Cartesian biology, and Maturana and Varela described it in 1981 as:
“a network of processes of production (transformation and destruction) of components which: (i) through their interactions and transformations continuously regenerate and realize the network of processes (relations) that produced them; and (ii) constitute it (the machine) as a concrete unity in space in which they (the components) exist by specifying the topological domain of its realization as such a network.”
While a cognitivist might recognize a consonance with cybernetics here, abandoning representationalism is very difficult for some. What other bridging concepts are there to relate brain and mind events? This is still an open issue.
As it turned out, a sophisticated alternative to cognitivism was on the way: Walter Freeman, Francisco Varela, and others have offered a post-representationalist approach to consciousness, cognition, and the brain based in dynamical systems theory. The undercurrents of dissatisfaction with understanding the mind as information-processing, rule-based symbolic logical procedures, and “computations over representations” emerged in the 1990’s as embodied cognitive science and neurophenomenology.
(Part I is here, and part III is here)
*-when asked about Understanding Computers and Cognition, a doctoral student in psychology I knew could only shake his head, raise his eyebrows, and say “that’s a weird book”